Days-old MDS creating chaos for some providers
DENVER — Just two days into a new era in nursing home patient assessments, providers were reporting widespread struggles with an updated MDS system, observers said Tuesday.
The new MDS 3.0 v1.18.11 makes more demands of staff time, and quicker action in many cases. Despite months of preparation, however, it is clear many hurdles still remain, experts told McKnight’s Long-Term Care News.
“[Electronic medical record] configuration issues are rearing their ugly head,” Celtic Consulting CEO Maureen McCarthy said. “Things that providers thought were all set to populate [in forms] have glitches.”
Other high-problem areas being reported early after the Oct. 1 transition include new interview sections regarding race and ethnicity questions, she added. Providers may no longer enter information about these and other social determinants without actually consulting patients.
“Folks were not aware that is needed to be completed prior to the assessment reference date, or within the first seven days of entry,” McCarthy added.
Perhaps a foreboding sign, she said that such lapses were occurring despite the fact that “there was plenty of education and guidance from CMS on that.”
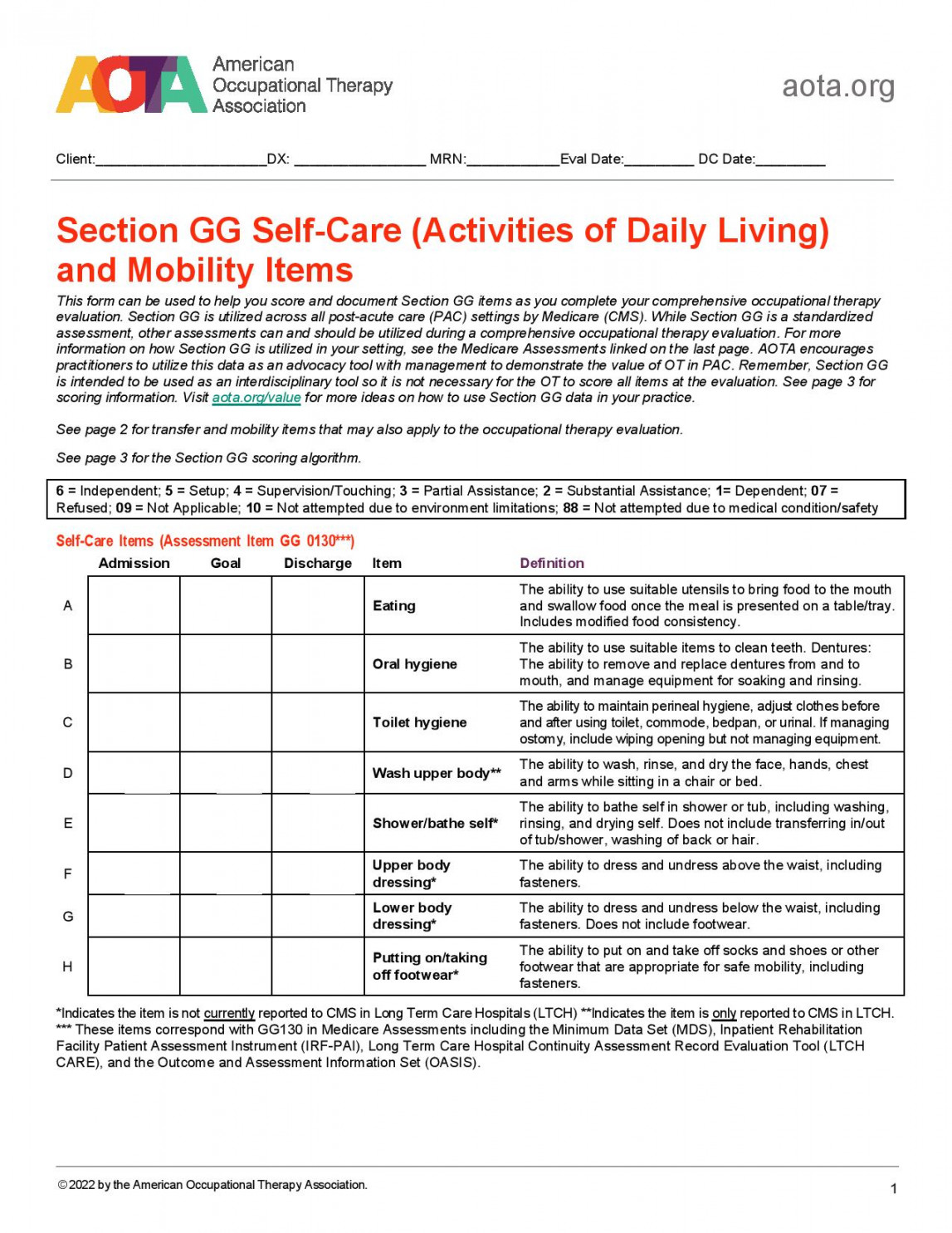
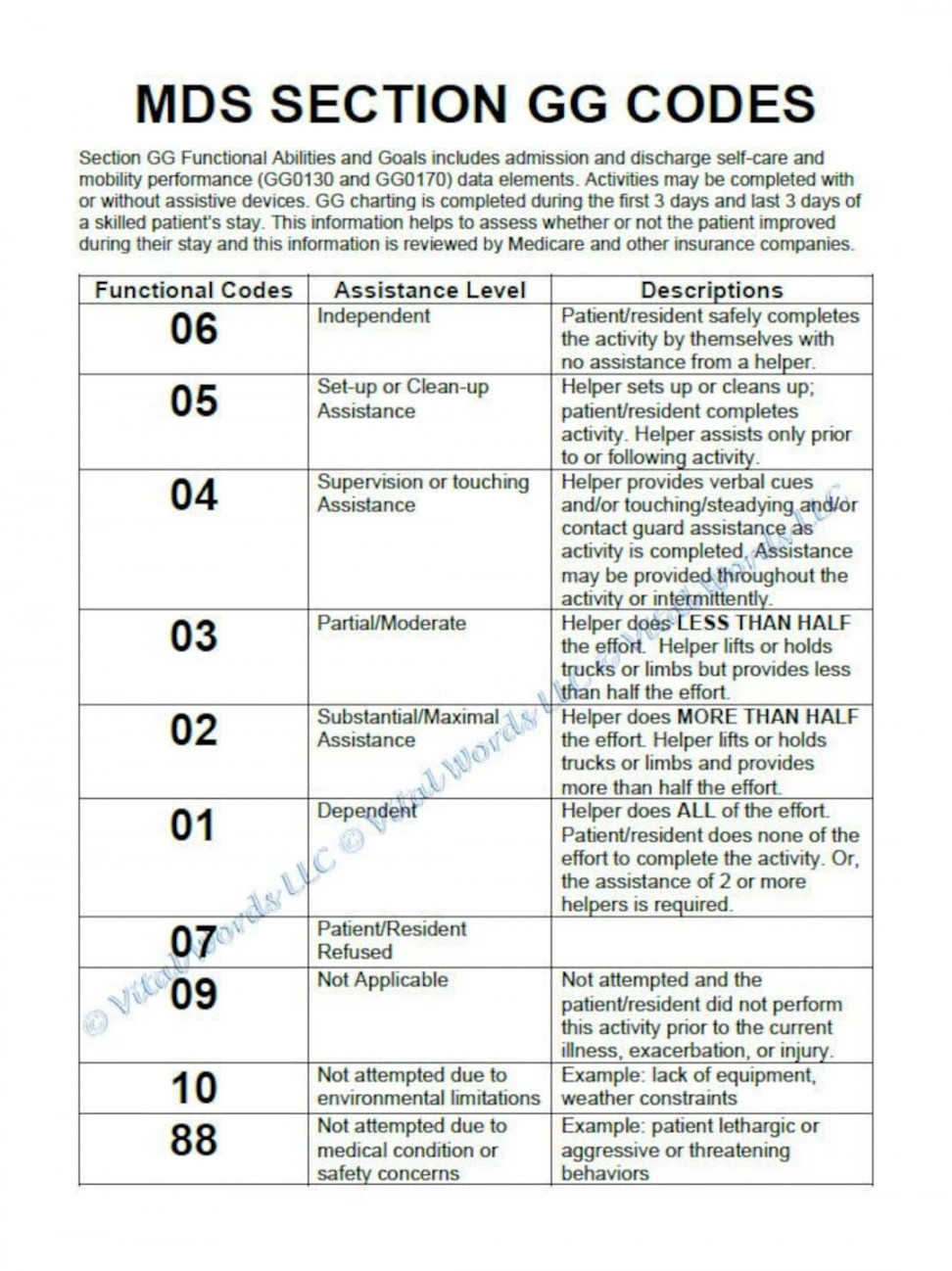
Of the many changes, she thinks provisions of the new Section GG represent “the biggest change globally.”
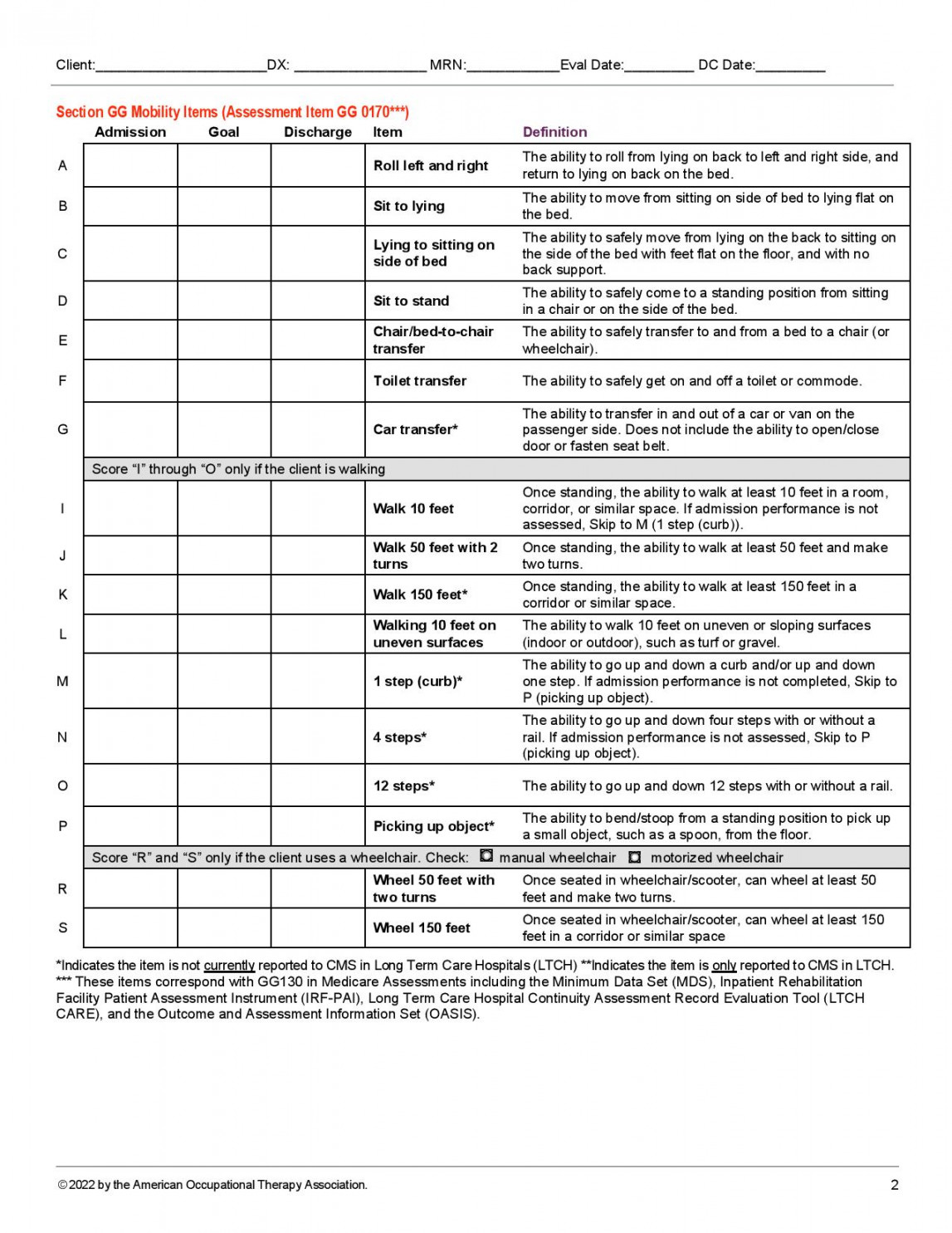
“It impacts more people in the building than any of the other changes do,” McCarthy explained. “So they’re always looking for what the other guy is doing, rather than looking for the best solution for their own situation. It amazes me that there are so many people here looking at how they’re going to manage GG and it’s already Oct. 1. It adds more stress to the entire process.”
Amy Stewart, chief nursing officer for the American Association of Post Acute Care Nursing, which specializes in nurse assessment education and coordination, said Tuesday that members were not reporting much about the new MDS. But problems seem “pretty widespread.”
“People are getting ‘fatal’ errors when trying to submit assessments,” she told McKnight’s. “There is also the issue of the deaths in facility requiring race and ethnicity (designations). That’s what we’re hearing. Those are resident-asked questions, and if the resident is dead, we can’t ask it again.”
Bigger MDS workloads
McCarthy was called on to provide a critical MDS update session at the American Health Care Association annual conference here. Among other points of emphasis, she planned to warn providers in her Tuesday afternoon session that more interdisciplinary team coordination will be needed, and that rehab, for example, should not be considered the sole lead in gathering data and making decisions.
Stewart, another multi-session speaker at the AHCA meeting, told McKnight’s that she feared many providers were not fully aware of the “workload issues” that the new MDS provisions created for nurse assessment coordinators and others such as as social workers and admissions, to name just a few..
“It might be surprising to some operators,” she said.
McCarthy noted that any changeover is bound to cause some problems, but she was concerned about the level of inactivity among some providers.
“It’s like they’re watching water go under the bridge so they can make changes after that,” she said with a shake of her head. “There’s uncertainty about how to put processes in place. Some are always looking for what the other guy is doing rather than doing it on their own.”
The risk in that, of course, is lost revenue, especially with a narrower, three-day lookback period that could already be biting some providers today if they weren’t primed to act given Sunday’s switchover. Later, there could be problems when regulatory reviews take place, she warned.
“So many people have an incomplete process,” for contending with new provisions, McCarthy said.
Three tips for success
She made three recommendations to providers still working to catch up:
Look at your intake documentation and forms. Make sure the intake forms have the information you need to support the new MDS. Get rid of old ones. Nursing departments must be sure they’re aware there is a process that goes along with the transfer of health information. “The expectation is we’re having a conversation with the resident, because I don’t think the [staff] are understanding that piece. It’s not just giving a piece of paper to the person. We really need to have the explanation about the medications they’re taking.” It has to be explained to the patient [or patient representative] or the next provider downstream. That all takes extra time. “I think it’s a great opportunity to improve care throughout the continuum,” she conceded. Have all three pieces necessary to support Section GG documentation, and have it reproducible: The data collection, the assessment and then the coding itself.
“That’s probably the lowest hanging fruit, I would say, and probably one of the first things that auditors would come after to try and reduce your revenue,” McCarthy warned.
“The majority [of providers] don’t have a full plan,” she reflected Monday. “Smaller facilities, and moms-and-pops are limping along. They face potential regulatory noncompliance problems — and the potential financial impact will hurt.”
McCarthy and other experts believe providers will be better off in the long term under the new system. But providers need to get new processes in place, as soon as possible.
“I would absolutely say it’s a chaotic time,” McCarthy said. “It reminds me of when we went from the MDS 2.0 to 3.0 in 2010. It reminds me very much of that. The one good thing we have in this system that we didn’t have in 2010 is we don’t need to do a new MDS for every single patient beginning Oct. 1.”